Pericarditis
Our article is about an important cause of chest pain; Pericarditis. Though it is not really as serious as angina pectoris, it can lead to bad complications if left untreated or not diagnosed in the early stages.
Definition of Pericarditis
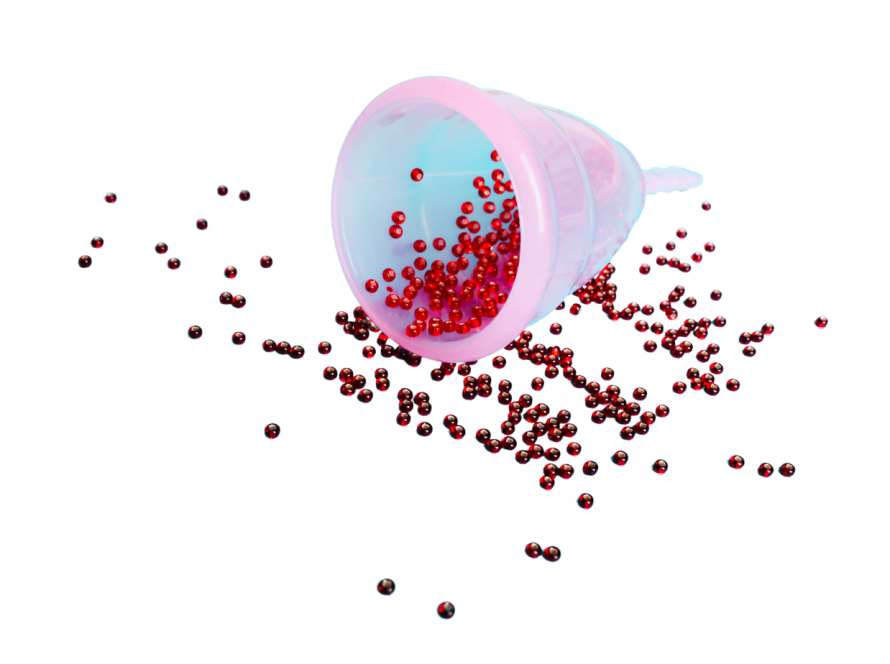
Pericarditis is inflammation and irritation of the pericardium, which is a thin, sac-like tissue that surrounds the heart. The pericardium has two layers which have a small amount of fluid between them. This fluid is to lubricate the heart. The pericardium helps to keep the heart in place inside the chest wall. Pericarditis can cause sharp chest pain and other symptoms that we will see below.
Symptoms
– Chest pain: which is the most common symptom of pericarditis. It is usually a sharp, stabbing pain. It occurs behind the breastbone or on the left of the chest. It gets worse while coughing, lying down, or taking a deep breath. It gets better while sitting up or leaning forward.
– Cough
– Fatigue
– Fever
– Heart palpitations
– Shortness of breath
Causes
Sometimes, doctors cannot determine the cause of pericarditis, and that is called idiopathic pericarditis. Causes can include:
– Heart surgery or heart attack
– Infection
– Systemic inflammatory diseases, such as rheumatoid arthritis or lupus
– Trauma
– Radiation treatment
– Other diseases may include kidney failure, tuberculosis, AIDS, or gout.
Risk Factors
The risk factors are the same as the causes above.
When to see a doctor?
As we always say, any patient with chest pain should seek medical advice as soon as possible. Because the sooner we diagnose the disease, the better the response to the treatment will be.
Diagnosis
– ECG: to see if there are changes that indicate pericarditis
– Serum troponin: to see if there is acute coronary syndrome or myocarditis
– Pericardiocentesis: to do lab tests on the pericardial fluid
– CRP: it can be elevated
– Full blood count: we can see elevated white blood cells
– Liver function tests: elevated if there is liver congestion
– Serum urea: to rule out the uremic cause
– Electrolytes
– Chest X-Ray
– Echocardiograph
– Autoimmune screen: to see if there is any immune disease
– Viral screen
– Chest CT or cardiac MRI
– Pericardial biopsy
Differential Diagnosis
– Pulmonary embolism
– Myocardial infarction
– Pneumonia
– Pneumothorax
– Costochondritis
Management
The treatment of pericarditis depends on the severity and the cause of the disease. Medications are often described to reduce swelling and inflammation.
– Medications can include:
– Colchicine
– Corticosteroids
– Pain relievers: such as Aspirin or Ibuprofen
If the cause of the pericarditis is bacterial, antibiotics will be described, and even drainage if necessary.
Most patients recover in two to four weeks.
· Surgery or other procedures:
– Pericardiocentesis: doctors use a sterile needle or small catheter to drain the excess fluid from the pericardium cavity.
– Pericardiectomy: in this surgery, we remove the entire pericardium.
References
Mayo clinic – BMJ – Healthline – WebMD – American Heart Association
If you have any concerns about non-emergent health conditions, you may schedule a telemedicine consult with Dr Kaako for individualized consultation.